Suicide Rates in the U.S.
Pre-COVID-19, suicide rates overall increased in the United States from 1999-2016. Suicide made the top-10 leading causes of death in every age group in 2019, with a concerning increase in younger age groups.
However, during 2020, suicide was knocked off the top-ten list by COVID-19, and actually decreased by 2,677 from the previous year.
“Fake News” in the early stages of the pandemic led hysterical rhetoric that there was a massive increase in suicide rates due to quarantine. One tweet in particular claimed a “200% rise” in suicide that was reposted 31,000 times before being taken down. Fake news aside, the data shows a slight decrease suicide during 2020, with an increase in anxiety & depressive disorder.

Anxiety Disorder & Depressive Disorder Rising
In a survey conducted by the CDC anxiety disorder and depressive disorder, risk factors for suicide ideation, has increased considerably in during April – June 2020, compared to the same period in 2019. This survey revealed that serious suicide ideation was higher among respondents age 18-24, minority racial/ethnic groups, self-reported unpaid caregivers for adults, and essential workers. Communities and healthcare professionals should be especially aware that prevention and intervention may be more prevalent among these groups.
Even though suicide rates across all age groups did not spike by 200%, 44,834 deaths and reported increase in serious suicide ideation among certain demographics is definitely a cause for concern among communities and health care professionals.
September is Suicide Prevention Month, marking an opportunity to review how we can all recognize and prevent suicide ideation in patients, friends, and family, and learn about tools to support prevention.
Warning Signs among friends, family, and people in your community:
Warning signs are often conveyed through conversations. Pay attention to the topics your friends or family talk about. Talking about wanting to die or kill themselves, feeling empty or hopeless, being a burden to others, feeling like they have no reason to live, or feeling trapped, without any solutions are all red flags of potential suicide ideation.
Acting reckless, giving away valuable possessions, and even going as far as saying goodbye to friends and family, or withdrawing from friends and family are also warning signs that you may need to intervene.
Other warning signs according to the NIH include displaying extreme mood swings, planning or looking for ways to kill themselves, talking about feeling great guilt or shame, using alcohol or drugs more often, acting anxious or agitated, changing eating or sleeping habits and showing rage or talking about seeking revenge.
Intervention #BeThe1To:
If you notice these warning signs, it’s time to implement this five-step intervention plan proposed by the #BeThe1 suicide prevention campaign.
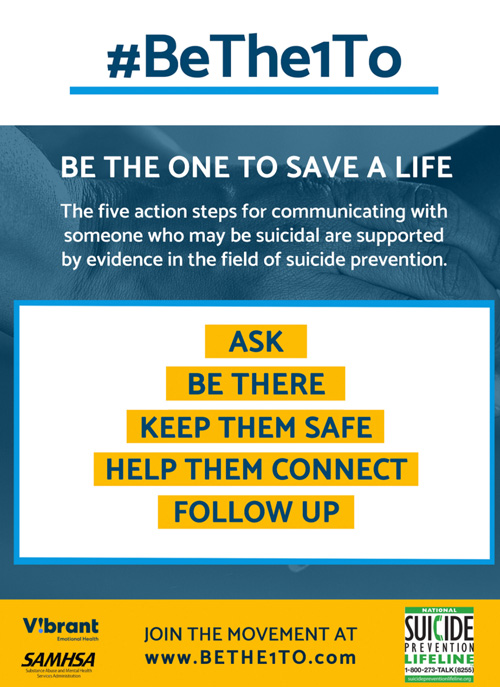
1. Ask “Are you thinking about killing yourself?”
2. Keep them safe, & reduce access to highly lethal items or places.
3. Be there, and listen carefully to acknowledge and talk about what that person is thinking and feeling.
4. Help them connect to the free and anonymous suicide prevention hotlines and chats listed below.
5. Stay connected afterwards, follow up and stay in touch with the person struggling with emotional pain.
Free and anonymous suicide prevention hotlines and chats.
These services are free and available 24 hours a day, seven days a week. All calls & texts are confidential.
National Suicide Prevention Lifeline 1-800-273-TALK (8255)
Crisis Text Line (text HELLO to 741741) Facebook messenger chat also available.
Veterans Crisis Line 1-800-273-8255 and Press 1. Chat also available.

Suicide Risk Evaluation in the ED
A study published in 2015 showed that universal screening all patients in the ED led to a nearly twofold increase in risk detection. Identifying risk is the first step in intervention. PEPID subscribers can utilize questionnaires, and open calculators to quickly identify high risk patients right at the point of care.
As a healthcare provider, risk of suicidality should never be considered zero. A previous suicide attempt is the single most important risk factor. Other risk factors include depressive disorder, severe anxiety, PTSD, Schizophrenia, bipolar disorder, personality disorders like borderline personality disorder, alcoholism, and substance abuse.
While you are assessing your patients, it’s best to start with subtler open-ended questions that are less serious, and gradually ask more targeted questions about suicide ideation. Determine the severity of the patient’s feelings, and elicit any specific plans for intent for suicide, including lethality and specificity of the ideation, and ask about whether or not the patient has access to these weapons.
Give more weight to the patient’s history, risk factors and collateral information than the patient let’s on since often a truly suicidal patient will not admit it. After interviewing the patient, prioritize risk factors by chronic or predisposing factors, then acute or exacerbating factors, followed by the presence of absence of protective factors like religion or motivations, and finally determine imminent risk of suicide.
The Suicide Risk Assessment monograph in PEPID Primary Care Plus Ambulatory Care Suite (also including in Emergency Medicine Suite) guides providers through the entire evaluation process.
Point-of-care Assessment Tools
Live interactive questionnaires are intuitively linked in the Suicide Risk Evaluation Assessment monograph to allow providers to input answers to pertinent questions right in the app or online portal to generate actionable answers in real time.
The SAD PERSON’s Assessment distinguishes if the patient is safe for discharge, in need of emergency psychiatric consultation, or requires hospitalization.
Evaluate a patient’s depression severity with the Patient Health Questionnaire, or PHQ-9 screening. This nine-question survey determines suggested depression severity from non-minimal to severe, a known risk factor for suicide.
Evaluate for any neurocognitive impairments with the mini-mental exam, mini-cog exam. Assess alcoholism with the CAGE questioning, and substance-abuse with the CRAFFT questionnaire.
Use the Suicide Ideation Scale to score a patient’s suicide ideation. This equation factors 19 points each weighted form 0-2. A low score from 0-19 suggests a low suicide ideation, while a score 19 or over suggests a high suicide ideation.
Access all of these live point of care tools with a free two-week trial if you are not already a PEPID subscriber.
When You Suspect Suicide Ideation
Early identification and management of suicide ideation works to prevent suicide. If a patient is ranking high for suicide ideation, depressive disorder, etc. refer them immediately to a psychiatry specialist. Encourage the patient or friends of the patient to limit their access to firearms, detoxification of domestic gas, and prescriptions drugs. Be prepared with community support groups in your area for patients to utilize. And finally, educate patients about the free and anonymous hotlines available to them 24/7 365 days a year.

Suicide Prevention in Healthcare Professionals
Suicide rates and burnout are higher among physicians than the general population. Physicians and trainees can experience mental distress and even PTSD while treating patients. Twenty-eight percent of residents experience a major depressive episode during training, which is a 20% higher rate than the general population of the same age group.
With the latest surge in hospitalized COVID-19 patients as the population battles the more contagious Delta variant, critical healthcare professionals are feeling increased anxiety, hopelessness, and PTSD. During this pandemic, healthcare professionals must recognize their stress, take steps to build resilience & healthy coping mechanisms, and get help when they need it.
Know where to go if you need help.
Physician Support Line is a national, free, and confidential support line service made up of 600+ volunteer psychiatrists, joined together in the determined hope to provide peer support for our physician colleagues and American medical students as we all navigate the COVID-19 epidemic. Call 1-888-409-0141
The Emotional PPE Project The Emotional PPE Project connects any healthcare worker impacted by the COVID pandemic with free confidential therapy by a volunteer therapist who wants to help.
The Disaster Distress Helpline, 1-800-985-5990, is a 24/7, 365-day-a-year, national hotline dedicated to providing immediate crisis counseling for people who are experiencing emotional distress related to any natural or human-caused disaster.
SAMHSA’s National Helpline Call 1-800-662-HELP (4357), is a confidential and free hotline providing resources on mental and substance use disorders including referrals to local treatment facilities, support groups, and community-based organizations in English and Spanish. Available 24/7.
CDC Tips to cope and enhance your resilience.
September 17: National Physician Suicide Awareness Day
Shine a Light. Speak its name.
In order to address the issue of physician suicide, the Council of Residency Directors in Emergency Medicine (CORD), in collaboration with AAEM, ACEP, ACOEP, EMRA, RSA, RSO, and SAEM have come together to annually dedicate September 17th as National Physician Suicide Awareness (NPSA) Day. Find out how to support the #NPSAday movement here.



Trackbacks/Pingbacks