While medical R&D has been making great strides in precision medicine and pharmacogenetics – ultimately tailoring diagnostics and treatments to match individuals on a submolecular level – healthcare providers need to remember that their relationships with their patients and patients’ families are evolving too.
Providers and policy-makers alike should take time to evaluate how the clinician-patient relationship is evolving, how it is being nurtured, and how clinicians can tap into one of the most underutilized resources (sometimes the greatest barrier) to health in modern medicine: the patient.
Every year about 3.8 billion prescriptions are written out to a patient population with an alarming rate of nonadherence to treatment. This costs the US about $100-$300 billion healthcare dollars annually, as poor adherence increases risk for hospitalization, readmission, and premature death – accounting for 125,000 deaths every year.1,5
While progress such as genetic testing for optimized treatments is a critical step towards improving patient outcomes, what use are medical and pharmacologic breakthroughs if the patients don’t even want to – much less, know how to take their pills? And with the time the average patient spends actively availing of healthcare (i.e. consulting with a primary care physician, visiting the ER, hospitalization) being a tiny blip within a long lifetime of relying on self-care and social support, how can healthcare providers make an impact? 3,6
Individualized treatments mean individualized patient needs. Are you and your team adding value to constrained patient interactions? PEPID highlights the importance of covering all 8 bases of the Picker Institute’s Principles of Patient-Centered Care. Defined by Harvard Medical School researchers as a truly holistic approach to personalized medicine, it positions patients as informed decision-makers and partners in their own healthcare.2
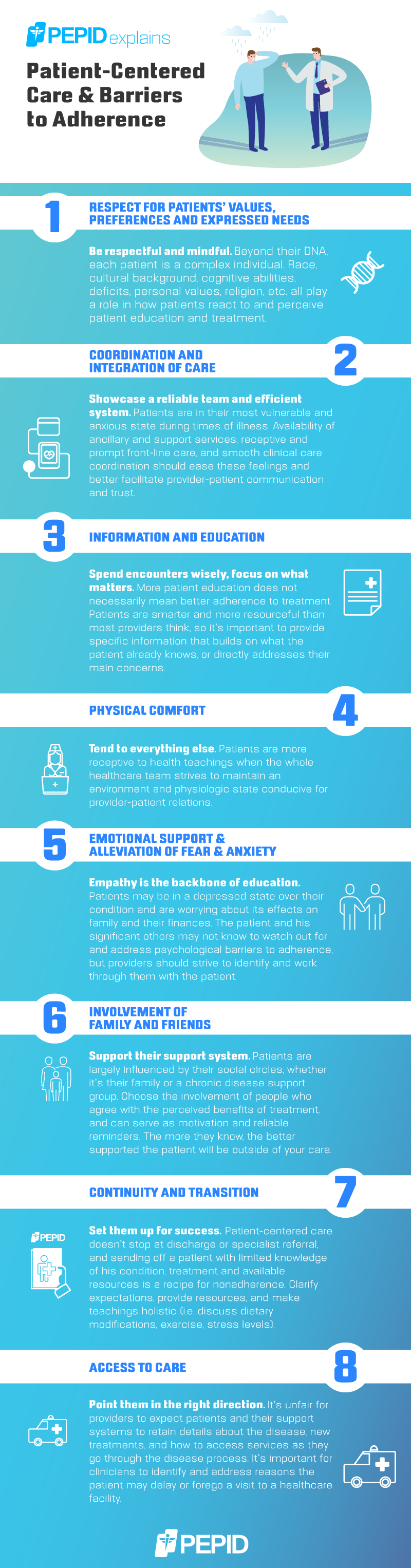
Nonadherence to treatment can certainly be costly and frustrating to healthcare providers, but our review of the Picker Institute’s 8 Principles of Patient-Centered Care shows there’s plenty of room for providers to meet patients in the middle. With the multitude of barriers arising between the time patients get prescriptions filled and their next appointment, and factoring in constantly shifting health plans and premiums, some doctors may never even see some of their patients again. When healthcare providers and their patients have a mutual respect and desire to learn from each other, true patient-centered care and optimal clinical outcomes are achieved.
Resources:
- “Benchmarks in Improving Medication Adherence.” The Healthcare Intelligence Network, 2010, http://www.hin.com/library/PreviewMedicationAdherenceBenchmarks.pdf.
- “The Eight Principles of Patient-Centered Care · Oneview.” Oneview, 1 Feb. 2018, https://www.oneviewhealthcare.com/the-eight-principles-of-patient-centered-care/.
- Chesanow, Neil. “Why Are So Many Patients Noncompliant?” Medscape Nurses, https://www.medscape.com/viewarticle/818850.
- Gold, Deborah T., and Betsy McClung. “Approaches to Patient Education: Emphasizing the Long-Term Value of Compliance and Persistence.” The American Journal of Medicine, Apr. 2006, https://www.amjmed.com/article/S0002-9343(05)01201-5/fulltext.
- Neiman AB, Ruppar T, Ho M, et al. CDC Grand Rounds: Improving Medication Adherence for Chronic Disease Management — Innovations and Opportunities. MMWR Morb Mortal Wkly Rep 2017;66. DOI: http://dx.doi.org/10.15585/mmwr.mm6645a2.
- Osterberg L, Blaschke T. Adherence to medication. N Engl J Med 2005;353:487–97.


Trackbacks/Pingbacks